

Monaco est une principauté située sur la Côte d’Azur et bordée par la mer méditerranée. Considéré comme le second plus petit état du monde (après le Vatican), Monaco est connue pour son style de vie luxueux, ses casinos haut de gamme et ses vues côtières spectaculaires. Malgré sa petite taille, tout en longueur, la Principauté de Monaco possède une histoire et une culture riches, et est notamment connue pour le Grand Prix de Monaco et le Rallye Monte-Carlo.
De son côté, la famille royale de Monaco, la Maison Grimaldi, est au pouvoir depuis le 13ème siècle. Le prince Albert II en est le souverain actuel, succédant à son père, le prince Rainier III, depuis le 6 avril 2005. Il est marié à la princesse Charlène, une ancienne nageuse olympique originaire d’Afrique du Sud, avec qui il a deux enfants, des jumeaux, la princesse Gabriella et le prince Jacques.
L’histoire de la royauté à Monaco
Comme indiqué en introduction, l’histoire de la royauté à Monaco remonte au 13ème siècle. En effet, c’est en 1297 que la famille Grimaldi a pris le contrôle de la région de Monaco. Depuis, la dynastie Grimaldi a été au pouvoir, faisant de Monaco l’une des plus anciennes monarchies au monde.
La dynastie des Grimaldi

Les Grimaldi sont une famille noble dont les origines remontent au 11ème siècle. Constituée de seigneurs génois, la famille Grimaldi a acquis du pouvoir et des richesses grâce à son activité commerciale en Méditerranée.
L’histoire raconte qu’en 1297, Francesco Grimaldi pris le contrôle du château de Monaco en se faisant passer pour un moine et en renversant les gardes. Cet événement est considéré comme la naissance de l’État monégasque, faisant de Francesco Grimaldi, le premier seigneur de Monaco.
Bien évidemment, au fil des siècles, et comme de nombreuses autres dynasties, la famille Grimaldi a connu des périodes d’instabilité et de guerre, mais également des périodes de prospérité et de développement économique. Ainsi, c’est au 19ème siècle que le prince Charles III a décidé de moderniser le pays, en construisant le premier casino de Monte-Carlo et en développant l’industrie touristique.
L’évolution de la royauté à Monaco
Malgré le fait que la royauté de Monaco ait une très longue histoire derrière elle, notons que c’est le mariage du prince Rainier III à la star hollywoodienne Grace Kelly qui a véritablement fait connaître les Grimaldi au niveau international. Aujourd’hui, c’est leur fils, le prince Albert II qui est le souverain à la tête de la monarchie.
Ce dernier continue le travail de ses ancêtres en développant l’économie, et en faisant de la principauté une destination touristique de renommée mondiale. De nos jours, la famille Grimaldi est connue dans le monde entier pour son style de vie luxueux et son engagement philanthropique.
Les membres de la famille royale monégasque
La dynastie Grimaldi s’est beaucoup agrandie à travers les siècles, et ce, grâce aux différents mariages et unions célébrés.
Le prince souverain Albert II de Monaco
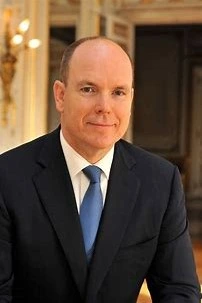
Le Prince Albert II de Monaco est né le 14 mars 1958 à Monaco, et est le fils du prince Rainier III et de la princesse Grace de Monaco. Malgré un début de carrière professionnelle dans le secteur financier, il a finalement décidé de revenir à Monaco pour se consacrer aux affaires de la principauté.
C’est en 2005 qu’il succède à son défunt père, devenant le nouveau souverain de la principauté.
Depuis, il s’est engagé dans de nombreux projets pour moderniser et développer Monaco, notamment dans les domaines de l’environnement, de l’éducation et de la recherche scientifique.
En 2011, le prince Albert a épousé Charlene Wittstock, une ancienne nageuse professionnelle sud-africaine, et le couple a depuis eu deux enfants, les jumeaux Jacques et Gabriella.
La princesse héritière Charlène de Monaco
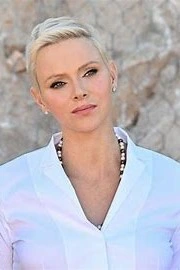
La princesse Charlène de Monaco, née Charlène Lynette Wittstock le 25 janvier 1978 en Afrique du Sud, est l’épouse du prince Albert II et la princesse héritière de Monaco.
En tant que nageuse professionnelle, Charlène Wittstock a remporté plusieurs titres nationaux et internationaux, et a également représenté l’Afrique du Sud aux Jeux olympiques de Sydney en 2000.
Ainsi, c’est en 2007 que Charlène rencontre le prince Albert II lors d’une compétition de natation à Monaco.
Le couple s’est ensuite fiancé en 2010, suivi d’un mariage largement médiatisé en 2011 puis de la naissance des jumeaux, en décembre 2014. La princesse Charlène est connue pour son style élégant et sa présence charitable, et est souvent comparée à la princesse Grace de Monaco pour sa beauté et son charisme.
Les enfants du couple princier
Le prince Jacques et la princesse Gabriella sont donc nés en décembre 2014 et sont les héritiers du trône de Monaco. Ainsi, le prince Jacques est l’aîné des jumeaux et est donc l’héritier direct du trône et la princesse Gabriella quant à elle, étant la cadette, occupe le deuxième rang dans l’ordre de succession.
Depuis leur naissance, les jumeaux ont été très présents dans la vie publique de Monaco, accompagnant souvent leurs parents lors d’événements officiels et de célébrations nationales.
Étant considérés comme les héritiers de la principauté, leur rôle futur en tant que souverains est très attendu. Néanmoins, pour le moment, ce sont encore des enfants insouciants, qui profitent de leur enfance, entourés de leur famille.
Les événements importants de la vie royale monégasque
La famille royale monégasque a eu une histoire longue et fascinante qui a été marquée par plusieurs événements importants. Des couronnements aux mariages, en passant par les naissances, ces événements ont joué un rôle essentiel dans le façonnement de l’histoire de Monaco et l’image de la famille princière.
Les mariages royaux
Les mariages royaux à Monaco sont des événements grandioses et très médiatisés. À titre d’exemple, le mariage du prince Albert II avec Charlène Wittstock en 2011 a été couvert par les médias du monde entier, avec des célébrités et des dignitaires de haut niveau qui ont assisté à la cérémonie.
Comme dans les mariages classiques, un mariage royal à Monaco se passe généralement en deux parties : un mariage civil et un mariage religieux. La partie civile est un événement assez intime, réservé aux membres de la famille et à un petit groupe d’invités.
Le mariage religieux quant à lui est un événement plus grandiose, avec une procession à travers les rues de la ville de Monaco et une cérémonie à la cathédrale de Monaco.
Les baptêmes et les cérémonies officielles
Les baptêmes et les cérémonies officielles à Monaco sont souvent des événements très médiatisés en raison de l’importance de la famille royale monégasque et de son influence dans le monde. Voici un tableau récapitulant des informations générales sur ces événements.
| Les baptêmes | Les cérémonies officielles |
|---|---|
| Les baptêmes des membres de la famille princière sont souvent célébrés dans la chapelle palatine du palais princier de Monaco. La cérémonie est généralement privée, mais les médias sont parfois autorisés à photographier les membres de la famille à l’extérieur de la chapelle avant ou après la cérémonie. Les noms des bébés sont souvent annoncés à l’occasion de ces événements. | Des cérémonies officielles sont organisées pour célébrer des événements importants tels que la fête nationale ou l’anniversaire de la naissance du prince Albert II. Ces cérémonies peuvent inclure des défilés, des feux d’artifice et d’autres événements publics. Les membres de la famille princière assistent généralement à ces événements et sont souvent photographiés ou filmés par les médias. |
Les fêtes nationales et les traditions monégasques
Comme de nombreux pays à travers le monde, la Principauté de Monaco célèbre plusieurs fêtes nationales. Parmi les plus importantes, nous pouvons citer :
- La Fête Nationale de Monaco : célébrée le 19 novembre, également appelée le « jour du souverain » ;
- La fête traditionnelle de Sainte-Dévote : chaque année, en date du 27 janvier, une grande célébration est organisée à la mémoire de sainte Dévote, patronne de Monaco.
En outre, Monaco célèbre également l’anniversaire du prince en mars, en plus de fêtes plus classiques, tel que le nouvel an.
Le rôle de la famille royale monégasque dans la société
Bien que la principauté soit devenue depuis 1911 une monarchie constitutionnelle, la famille royale joue un rôle très important et essentiel dans la vie sociale monégasque.
En effet, cette dernière est une véritable source d’inspiration et un modèle pour les habitants, respectée et appréciée par toute la population. Mais pour obtenir cette admiration, la famille royale doit aussi se plier à de nombreuses obligations et interdictions. Ainsi, la principale fonction de la famille royale est avant tout de gouverner le pays et de le protéger, en collaboration avec le gouvernement et le parlement.
Le soutien aux associations caritatives et humanitaires
La famille royale de Monaco est très connue pour son travail philanthropique, notamment dans les domaines de la conservation de l’environnement et du développement durable. Ainsi, elle s’engage dans des programmes et associations pour favoriser l’accès à l’éducation et à la santé, et travaille en partenariat avec des fondations pour soutenir des initiatives liées à l’environnement.
La promotion de l’image de Monaco à l’étranger
Le rôle de la famille royale dans la représentation de Monaco à l’étranger est très important. En effet, la famille princière est le principal ambassadeur du pays et ses actions et décisions internationales sont largement médiatisées, ce qui contribue à augmenter la notoriété de Monaco à l’étranger.
De plus, la famille royale participe également à des événements et manifestations culturelles et sportives, ce qui permet de renforcer le dynamisme et la renommée du pays.
Par ailleurs, le travail diplomatique des membres de la famille royale contribue à tisser des relations avec des pays étrangers et à promouvoir les intérêts de Monaco sur la scène internationale. Enfin, notons que le fait que la famille princière bénéficie d’une large couverture médiatique, permet d’accroître la visibilité de Monaco partout dans le monde.
Les engagements politiques de la famille royale
En termes d’engagement politique, la famille royale monégasque contribue à :
- Promouvoir et soutenir la paix, la liberté et la tolérance au sein de la principauté ainsi qu’à l’international ;
- Développer des initiatives pour moderniser et renforcer les liens entre Monaco et ses pays voisins proches et lointains ;
- Préserver et encourager les activités sociales, culturelles et sportives, tout en s’engageant à promouvoir des valeurs fondamentales telles que la santé et l’environnement ;
- Renforcer l’idée de solidarité et de justice entre les citoyens et garder le respect des droits fondamentaux ;
- Protéger et préserver l’héritage culturel et historique de Monaco ;
- Protéger la biodiversité et la beauté naturelle de la principauté.
- Faire preuve de leadership pour le développement durable et à long terme.
- Défendre et promouvoir la philosophie monégasque et les principales valeurs-clés de la principauté.
Conclusion
Pour conclure, nous pouvons dire que l’avenir de la royauté monégasque est très prometteur. En effet, le prince Albert II, qui monte sur le trône en 2005 après le décès de son père, le prince Rainier III, démontre que la famille royale poursuit toujours sa mission de gouvernance et de progrès pour Monaco.
En effet, cette dernière favorise le développement économique du pays, notamment dans le tourisme, sa principale source de revenus. De plus, le prince cherche également à renforcer les liens entre les institutions monégasques et leurs communautés, ainsi qu’à enrichir la vie monégasque par le biais de manifestations culturelles et/ou sportives.
Enfin, notons que sa stratégie d’ouverture à l’étranger et aux médias a fait de Monaco un état modèle en matière de transparence et de modernité.
